-
The Future Of Nano Technology
Categories
- Ai
- Alan Watts
- Anatomy
- Andropause
- Anti-Aging Medicine
- Arthritis
- Artificial General Intelligence
- Artificial Intelligence
- Artificial Super Intelligence
- Ataxia
- Autism
- Biochemistry
- BioEngineering
- Biotechnology
- Bitcoin
- Chemistry
- Cryonics
- Cryptocurrency
- David Sinclair
- Dementia
- Diet Science
- Diseases
- Eczema
- Elon Musk
- Futurism
- Gene Medicine
- Gene Therapy
- Gene therapy
- Genetic Medicine
- Genetic Therapy
- Global News Feed
- Healthy Lifestyle
- Healthy Living
- HGH Physicians
- Hormone Optimization
- Hormone Replacement Therapy
- Hormone Replacement Treatment
- Human Genetic Engineering
- Human Immortality
- Human Longevity
- Human Reproduction
- Hypogonadism
- Hypopituitarism
- Hypothyroidism
- Immortality
- Immortality Medicine
- Inflammation
- Injectable Growth Hormone
- Integrative Medicine
- Life Skills
- Longevity
- Longevity Medicine
- Low T
- Machine Learning
- Mars Colony
- Medical School
- Menopause
- multiple-sclerosis
- Nano Medicine
- Nanomedicine
- Nanotechnology
- Neurology
- Parkinson's disease
- Pharmacogenomics
- Protein Folding
- Psoriasis
- Quantum Computing
- Regenerative Medicine
- Resveratrol
- Sermorelin Physicians
- Singularity
- Spacex
- Stem Cell Therapy
- Stem Cells
- Stemcell Therapy
- Testosterone
- Testosterone Physicians
- Transhuman
- Transhumanism
- Transhumanist
- Uncategorized
- Veganism
- Vegetarianism
- Vitamin Research
- Wellness
-
Recent Posts
- Cheap longevity drug? Researchers aim to test if metformin can slow down aging : Shots – Health News – NPR
- The U.S. Needs to ‘Get It Right’ on AI – TIME
- Big Tech keeps spending billions on AI. There’s no end in sight. – The Washington Post
- Racist AI Deepfake of Baltimore Principal Leads to Arrest – The New York Times
- A Baltimore-area teacher is accused of using AI to make his boss appear racist – NPR
Archives
Popular Key Word Searches
- centraltph
- bicarbonate and growth immunity ray peat
- vrcc neurology
- bibliotecapleyades/amrita-longevity-immortality
- cbr xmen anatomy
- Medical genetics wikipedia
- immortality medicine
- GrabPay
- Grab Pay Philippines
- GrabPay Vietnam
- GrabPay Philippines
- dr weil psoriasis
- what does recovered mean covid-19
- tony pantalleresco
- tony pantalleresco herbalist book
- herbsplusbeadworks
- herbsplusbeadworks website
- hailie vanderven
- princeton longevity center scam
- aetna genetic testing policy
- anatomy of hell
- biggie
- longevity claims
- augmentinforce tony pantalleresco
- tony pantalleresco website
| Search Immortality Topics: |
Category Archives: Nano Medicine
Scientists grow human mini-lungs as animal alternative for nanomaterial safety testing – The University of Manchester
Using the same biological endpoints, the teams human lung organoids showed a similar biological response, which validates them as tools for predicting nanomaterial driven responses in lung tissue.
The human organoids enabled better understanding of interactions of nanomaterials with the model tissue, but at the cellular level.
Graphene oxide (GO), a flat, thin and flexible form of carbon nanomaterial, was found to be momentarily trapped out of harms way in a substance produced by the respiratory system called secretory mucin.
In contrast, MWCNT induced a more persistent interaction with the alveolar cells, with more limited mucin secretion and leading to the growth of fibrous tissue.
In a further development, Dr Issa and Vranic based at the Universitys Centre for Nanotechnology in Medicine are now developing and studying a ground-breaking human lung organoid that also contains an integrated immune cell component.
Dr Vranic said: With further validation, prolonged exposure, and the incorporation of an immune component, human lung organoids could greatly reduce the need for animals used in nanotoxicology research.
Developed to encourage humane animal research, the 3Rs of replacement, reduction and refinement are now embedded in UK law and in many other countries.
Public attitudes consistently show that support for animal research is conditional on the 3Rs being put into practice.
Professor Kostas Kostarelos, Chair of Nanomedicine at the University said: Current 2D testing of nanomaterials using two-dimensional cell culture models provide some understanding of cellular effects, but they are so simplistic as it can only partially depict the complex way cells communicate with each other.
It certainly does not represent the complexity of the human pulmonary epithelium and may misrepresent the toxic potential of nanomaterials, for better or for worse.
Though animals will still be needed in research for the foreseeable future, 3D organoids nevertheless are an exciting prospect in our research field and in research more generally as a human equivalent and animal alternative.
Posted in Nano Medicine
Comments Off on Scientists grow human mini-lungs as animal alternative for nanomaterial safety testing – The University of Manchester
Histopathological biomarkers for predicting the tumour accumulation of nanomedicines – Nature.com
Quantification of the accumulation of nanomedicine in tumours
We first determined nanomedicine tumour accumulation in three mouse models with differing degrees of vascularization, stroma composition and target-site localization (Fig. 1a). The tumour models were A431 human epidermoid carcinoma, MLS human ovarian carcinoma and CT26 murine colon cancer. As a nanocarrier, we employed a 67kDa-sized poly(N-(2-hydroxypropyl) methacrylamide) (PHPMA) polymer, as this prototypic albumin-sized macromolecule has consistently provided us with high levels of tumour accumulation in a variety of models15,16,17. We used fluorescence reflectance imaging (FRI) and hybrid CTFMT to visualize and quantify the biodistribution and tumour accumulation of DY750-labelled PHPMA (Fig. 1b,c and Supplementary Fig. 1). When normalized to average tumour volume at the timepoint of analysis (250 mm3), at 72h post intravenous (i.v.) injection, we found average levels of target-site localization of 5.01.7, 8.51.6 and 10.21.7 percent of the injected dose (%ID) for A431, MLS and CT26 tumours, respectively, exemplifying sustained localization to tumours over time, as well as different accumulation patterns in the three models (P=0.0024, one-way analysis of variance (ANOVA); Fig. 1d and Supplementary Fig. 1). The tumours were then excised, and DY750-labelled PHPMA accumulation patterns were validated ex vivo using FRI (Supplementary Fig. 2). The collected tumours were fixed, sectioned and stained for biomarker assessment.
a, A schematic of the experimental protocol aimed at identifying tumour-tissue biomarkers that correlate with nanomedicine accumulation in tumours. The tumour accumulation of the prototypic polymeric nanocarrier, PHPMA, was assessed using CTFMT in three distinct mouse models with varying degrees of tumour targeting. Subsequently, correlation analyses were conducted using 23 tumour-tissue microenvironment features associated with tumour-targeted drug delivery, focusing on aspects related to the vasculature (red), stroma (green), macrophages (blue) and cellular density (grey). The dashed lines indicate double stained features. For further details, please refer to Supplementary Table 1. The illustration was created with BioRender.com. b, FRI-based, longitudinal optical imaging of DY750-labelled PHPMA accumulation in the tumours of mice with A431, MLS and CT26 tumours representing low, medium and high levels of target-site accumulation, respectively (the white dashed circles indicate tumour location, and one mouse per tumour model is shown). c,d, Longitudinal CTFMT visualization (c) and quantification of DY750-labelled PHPMA tumour accumulation (d) in percent of the injected dose (100% is equal to 2nmol of dye) normalized to 250mm tumour volume. The statistical significance between the two models was assessed via individual Students t-tests (A431 versus MLS, *P=0.0168; A431 versus CT26, **P=0.0025) and between all models via one-way ANOVA (#P=0.0024). Each data point represents a CTFMT scan of one animal.
We analysed 23 tumour microenvironment features associated with tumour-targeted drug delivery (Supplementary Table 1). These included vascular features, such as vessel density (CD31), perfusion (lectin) and angiogenesis (VEGFR2); lymph vessels (LYVE-1); extracellular matrix components, such as SMA, collagen I and collagen IV; tumour-associated macrophages (TAM; F4/80); and tumour cell density (4,6-diamidino-2-phenylindole). In addition, we analysed combinations of the above, via immunofluorescent double-stainings, to, for example, assess vessel support (SMA+/CD31+), vessel function (lectin+/CD31+) and the fraction of angiogenic vessels (VEGFR2+/CD31+).
The tumour-tissue biomarkers were captured and quantified via fluorescence microscopy and correlated with nanocarrier accumulation in A431, MLS and CT26 tumours (Fig. 2). Regarding blood vessel density and perfusion, we observed an overall good agreement between the number of (perfused) vessels and DY750-labelled PHPMA accumulation. The CT26 tumours had the highest number of total and functional blood vessels (89.035.9 and 48.018.8, respectively; Fig. 2a,b,g,h), and this was in line with their high level of polymer accumulation (10.21.7%ID per 250mm3; Fig. 1d). Conversely, A431 tumours had low levels of total and functional blood vessels (28.515.1 and 25.615.5, repectively; Fig. 2a,b,g,h), aligning with their low accumulation of DY750-labelled PHPMA (5.01.7%ID per 250mm3; Fig. 1d). Interestingly, while CT26 tumours had the highest absolute numbers of total and functional blood vessels, A431 tumours presented with the highest relative level of perfused vessels (91.3%, as compared with 62.7% for MLS and 54.9% for CT26; Supplementary Fig. 3j). This indicates that the absolute number of (functional) blood vessels is a more important factor determining nanomedicine tumour targeting than the relative fraction of vascular perfusion. In good agreement with this, also the absolute numbers of SMA+, Col I+, Col IV+ and VEGFR2+ blood vessels (Fig. 2c,d,i,j) correlated better with DY750-labelled PHPMA tumour accumulation than the relative fractions of SMA+, Col I+, Col IV+ and VEGFR2+ vessels (Supplementary Fig. 3jn).
af, Immunofluorescence stainings for all blood vessels (CD31) (a), actively perfused vessels (lectin) (b), pericyte-supported vessels (SMA) (c), angiogenic vessels (VEGFR2) (d), lymphatic vessels (LYVE-1) (e) and TAM (F4/80) (f) in A431, MLS and CT26 tumours. Scale bar, 50m. gl, Quantification of the immunofluorescence images for CD31+ vessels (g), lectin+ vessels (h), SMA+ vessels (i), VEGFR2+ vessels (j), LYVE-1+ vessels (k) and F4/80 (l) (no., number). The black bars indicate means. *P<0.05, **P<0.01 (Students t-test). Note that the analysis in gi is based on 10 magnification images, while the analysis in jl is based on 20 magnification. mr, Correlation of PHPMA tumour accumulation at 72h post injection (in percent of the injected dose (100% represents 2nmol of dye) normalized to 250mm tumour volume) with the respective tumour-tissue biomarker features (CD31+ vessels (m), lectin+ vessels (n), SMA+ vessels (o), VEGFR2+ vessels (p), LYVE-1+ vessels (q) and F4/80 (r)). The trendlines are shown per tumour model (colour-coded) and for all tumours together (black). The R2 values indicate the coefficient of determination and reflect the goodness of fit. Each data point represents one animal.
Regarding the retention component of nanomedicine tumour targeting, we particularly looked at LYVE-1+ lymphatic vessels and F4/80+ TAM. Interestingly, we observed that the tumour model with the highest level of PHPMA accumulation, that is, CT26, had almost double the number of LYVE-1+ lymphatic vessels as A431 and MLS (Fig. 2e,k). This indicates that the absence of effective lymphatics as a mediator of nanomedicine retention in tumours may be less important than originally anticipated18. It actually even suggests the opposite, which is that a certain degree of functional lymphatics in tumours may be needed to assist in attenuating the high interstitial fluid pressure that is typical of tumours19. A very good correlation was found between the density of TAM and nanomedicine accumulation (Fig. 2f,l,r). The area fraction of TAM increased from 2.2% to 5.1% to 7.7% for A431, MLS and CT26 tumours, respectively, correlating almost linearly with the increased tumour accumulation in these models (Fig. 1d) and resulting in good R2 values both within and across the three models (Fig. 2r). This finding corroborates an increasing number of notions that TAM act as a key reservoir for nanomedicine retention in tumours8,20. It furthermore implies that TAM density seems to be a suitable tumour-tissue biomarker to predict nanomedicine tumour accumulation.
Feature importance was assessed using gradient tree boosting (GTB). GTB is a machine learning technique for building predictive regression models based on a set of yes/no decision trees21,22,23. The trained GTB model considered all 23 features analysed as a regression model and was applied to predict polymeric nanomedicine tumour accumulation (Fig. 3a). Given the relatively small dataset, the leave-one-out method was employed to avoid the mixing of training and testing datasets. Ten decision trees, with a depth of up to eight questions, were found to be able to properly predict nanocarrier tumour accumulation based on histopathological features (R=0.70; Fig. 3b). As exemplified in Fig. 3c, GTB-based importance assessment identified the percentage of lectin+ (that is, functional vessels percentage) and angiogenic (that is, VEGFR2 vessels percentage) blood vessels, the density of TAM (that is, F4/80 area fraction (AF)) and the total, SMA+ and Col I+ number of blood vessels (that is, CD31 number, SMA number and Col I vessels number, respectively) as predictive features.
a, Schematic workflow. Tumour-tissue biomarkers were stained, quantified and correlated with the tumour accumulation of PHPMA nanocarriers. GTB-based machine learning was employed to rank feature importance using predicted versus measured PHPMA tumour accumulation values (Y, yes; N, no; B14, biomarker 14). b, N-fold cross-validation of predicted versus measured PHPMA tumour accumulation patterns illustrates the accuracy of the employed GTB method for predicting nanomedicine tumour targeting (in percent of the injected dose (100% represents 2nmol of dye) normalized to 250mm tumour volume). c, Ranking of the importance of the identified tumour-tissue biomarker features based on their assignment in the GTB decision trees (%, biomarker positive vessels of the number total vessels; no., number). The error bars indicate the standard deviaitoin (n=14).
When aiming to establish a biomarker for patient stratification, the practicality of the approach and the presence of a proper dynamic range are crucial. This implies that in the features identified via GTB, the functionality of tumour blood vessels needs to be excluded, because lectin cannot be injected in patients. For the fraction of VEGFR2+ blood vessels, the dynamic range is small (Supplementary Fig. 3l), making it unlikely to serve as a good biomarker. Moreover, as for the number of SMA+ and Col1+ blood vessels, double-staining would be required. This can be done preclinically with immunofluorescence, but is not typically performed in histopathological protocols in routine clinical practice. In follow-up studies with additional tumour models, we therefore focused on blood vessel and TAM density as tissue biomarkers.
The feature importance and biomarker potential of tumour blood vessels and TAM were confirmed in a panel of ten tumour models. This panel was selected to encompass models with very different tumour microenvironment architectures (thereby reflecting the heterogeneity observed in human tumours24) and consisted of six PDX and four CDX xenograft models. To ensure broad applicability of blood vessel and TAM density as biomarkers for predicting nanomedicine accumulation, we decided to employ a second drug-delivery system in these ten models, replacing the prototypic polymeric nanocarrier PHPMA with a PEGylated liposome formulation similar to Doxil/Caelyx25. Initially, fluorescent DiI-labelled liposomes were used to visualize the accumulation and distribution of liposomes in tumours. The highest levels of liposome accumulation were observed in E35CR and Calu-3 tumours, and the lowest levels were found in A549 and Calu-6 tumours (Fig. 4a).
a, Fluorescence microscopy analysis of Dil-labelled PEGylated liposomes (in red) in ten tumour models at 24h after i.v. administration Scale bar, 200m. The blood vessels are stained in green and the cell nuclei in blue. b, Tumour accumulation of PEGylated liposomal DXR in six PDX (green dots) and four CDX (red dots) tumour models. Individual and mean (black bars) tumour concentrations of DXR are shown for 20 mice per group and 5 mice per timepoint. c, Total tumour accumulation over time of PEGylated liposomal DXR (that is, AUC0120h). Values represent meanstandard error of the mean. d, Histopathological DAB staining of tumour blood vessels (CD31) and TAM (F4/80) for the ten models. Scale bars, 100m. eh, Quantification of blood vessel (e) and TAM (g) density based on DAB staining and correlation of blood vessel (f) and TAM (h) density with total liposomal DXR tumour accumulation (no., number of vessels or TAM per field of view).
We next used doxorubicin (DXR)-loaded liposomes and determined drug accumulation in tumours using high-performance liquid chromatography. For each of the ten models, this was done for four timepoints, with five tumours per timepoint (Fig. 4b). Total DXR concentrations over time were quantified and expressed as the area under the curve (AUC). In good agreement with the DiI-liposome fluorescence data (Fig. 4a), AUC determination demonstrated that tumour DXR concentrations were highest in E35CR and Calu-3, making these the highest drug-accumulating models, with drug levels three to five times higher than those of the majority of other models (Fig. 4c). A549 and Calu-6 were again found to accumulate the lowest amounts of liposomes, with DXR concentrations five to ten times lower than most other models. Interestingly, when comparing all AUC values together, it was furthermore found that PDX models presented with higher overall levels of liposomal DXR accumulation than CDX models (Fig. 4c).
In clinical practice, pathology protocols involve light (and not fluorescence) microscopy. Accordingly, we switched to 3,3-diaminobenzidine (DAB) staining and studied blood vessel and TAM density via standard histopathology in the ten PDX and CDX models. As shown in Fig. 4dh, we found that the three models with the lowest accumulation levels upon administration of liposomal DXR, that is, SW620, A549 and Calu-6 models (Fig. 4c), also presented with the lowest levels of CD31 and F4/80 staining. Across the ten different tumour models, there was a good correlation between tumour blood vessel and TAM density and nanomedicine accumulation (Fig. 4f,h). It should be noted in this regard, however, that the E35CR model was identified as a clear outlier, as it presented with the highest levels of Dil- and DXR-loaded liposome accumulation (Fig. 4ac), while its levels of CD31+ blood vessels were intermediate (Fig. 4f) and those of F4/80+ TAM were very low (Fig. 4g). When determining the area fraction of CD31 and F4/80 instead of the number of CD31+ and F4/80+ cells, observations were identical for all of the above notions, confirming the robustness of the tumour-tissue biomarkers identified (Supplementary Fig. 4). Altogether, these results demonstrate that there is a good correlation between the levels of the tumour blood vessels and TAM and the level of nanomedicine tumour accumulation.
Having identified tumour blood vessels and TAM as key features correlating with nanomedicine tumour accumulation, we next explored the robustness, validity and potential clinical applicability of combined tumour blood vessel and macrophage scoring, with the aim of developing a simple and straightforward biomarker protocol for patient stratification. This protocol is primarily designed to help predict which individuals from a heterogeneous patient population should be excluded in clinical trials, because their tumours are likely to show low nanomedicine accumulation and poor therapeutic efficacy (Fig. 5a).
a, Schematic workflow demonstrating the concept of patient stratification in cancer nanomedicine clinical translation based on tumour-tissue biopsies, created with BioRender.com. b, DAB staining illustrating the density of tumour blood vessels (CD31) and TAM (F4/80) in tumours, reaching from lowest (score 1) to highest (score 4) levels of blood vessel and macrophage density. Biomarker scores indicate 1 for absent, 2 for low, 3 for intermediate and 4 for high. Scale bars, 100m. c, Colour-coded heatmap, representing the distribution of CD31 and F4/80 product scores in the ten PDX and CDX tumour models with differing degrees of PEGylated liposomal DXR tumour accumulation. Tumours are ranked from high to low AUC, from top to bottom. Tumour-tissue biomarkers were scored by ten blinded observers, who each analysed three tissue sections per tumour model (n=30 in total). The colour intensity reflects the number of product scores. d, Schematic displaying the distribution of true and false positives and negatives in the tumour-tissue biomarker product score heatmap. e, Receiver operating characteristic (ROC) curve, generated on the basis of the tumour-tissue biomarker product scores, exemplifying very high diagnostic accuracy differentiating between low and high nanomedicine tumour accumulation (ROC curve is based on the scores in c; the red dashed line represents randomness and the units of the axis are in %).
We conceived a DAB-based histopathological scoring setup in which we considered 1 for absent, 2 for low, 3 for intermediate and 4 for high for the expression of both tumour-tissue biomarkers (Fig. 5b). Ten blinded observers, including three board-certified pathologists, were asked to score 60 tumour sections (30 for CD31 and 30 for F4/80; 6 for each tumour model). As shown in Fig. 5c, the colour-coded scoring intensities demonstrate that for tumour models with low CD31 and F4/80 product scores, the levels of liposomal DXR accumulation were also low. With a cut-off score of 6 to differentiate between tumours with low versus high nanomedicine accumulation, the blinded observers product scores correctly identified SW620, A549 and Calu-6 as true negatives (Figs. 4ac and 5c,d). Conversely, six out of seven models with good nanomedicine accumulation were correctly identified as true positives (Fig. 5c, d). The E35CR model turned out to be false negative, as its low CD31 and F4/80 product score incorrectly indicated that it would not accumulate liposomes well, which it clearly did do (Fig. 4ac). No false positives were detected (Fig. 5c,d). Altogether, nine out of ten tumour models could be correctly associated with low versus high nanomedicine accumulation on the basis of our tumour blood vessel and TAM biomarker product score.
To quantify the biomarker performance of our product score, we determined the area under the receiver operating characteristics (AUROC) curve. The AUROC curve represents a probability assessment, with a value of 0.5 resulting in a straight 45-line reflecting randomness (represented by the dashed red line in Fig. 5e). The AUROC curve represents the capability of a biomarker to distinguish between different classes, in this case between low versus high nanomedicine tumour accumulation. We obtained an AUROC value of 0.91 for our blood vessel and TAM product score (Fig. 5e), which is generally considered excellent for predicting nanomedicine tumour targeting, following the published criteria26.
The robustness and translatability of our biomarker product score were assessed in immunocompetent mouse models and in patient samples. The former were included to rule out the possibility that the presence of T cells plays an important role in determining nanomedicine delivery to tumours. To this end, we analysed PHPMA accumulation in orthotopic 4T1 triple-negative breast cancer tumours in BALB/c mice and PEGylated liposome accumulation in subcutaneous and orthotopic Hep55.1C liver tumours in C57BL/6J mice. As shown in Supplementary Fig. 5, good correlations between blood vessel and TAM product scores and nanomedicine tumour targeting were observed, as exemplified by R2 values of 0.51, 0.86 and 0.63, respectively. This confirms that our biomarker product score remains valid in syngeneic and orthotopic tumours in immunocompetent mice.
Next, we aligned our biomarker product score with the most comprehensive clinical dataset available on nanomedicine tumour targeting in patients27. In this study, the researchers used 111In-labelled PEGylated liposomes and quantitative SPECT imaging to assess nanomedicine tumour accumulation in 17 patients with different type of tumour27. For the most prevalent tumour types included, that is, ductal breast cancer, squamous cell carcinoma of the lung and squamous cell head and neck cancer, we collected matching tumour resection samples as well as primary tumour biopsies from the Biobank archive of the Institute of Pathology at RWTH Aachen University Hospital (Supplementary Table 5). Blood vessel (CD31+) and TAM (CD68+) density were analysed in ten different patient samples for each of the three cancer types, always in five different microarray sections for each individual tumour specimen. The expression levels and patterns of F4/80 and CD68 on TAM were demonstrated to be similar (Supplementary Fig. 6). Representative CD31 and CD68 stainings for breast, lung and head and neck cancer lesions are shown in Fig. 6a,b. Using QuPath software28, we quantified blood vessel and TAM density in these tumours and found that breast cancer typically presents with much lower levels of both tumour-tissue biomarkers as compared with lung and head and neck cancer (P<0.001 and P<0.0001 for blood vessels and P<0.05 for TAM; Fig. 6c,d).
a,b, Representative DAB stainings of blood vessels (a) and TAM (b) in tumour tissues obtained from patients with breast, lung and head and neck (H&N) cancer (all data in this figurre are based on tumour resections, and the data based on biopsies are shown in Supplementary Fig. 7). c,d, Quantification of blood vessels (c) and TAM (d) in ten patient samples for each tumour type (no., number per field of view; significance is indicated in P values based on Students t-test). e, Tumour accumulation of 111In-labelled PEGylated liposomes in patients with breast, lung and head and neck (H&N) cancer (in percentage of the injected dose per kilogram tumour). The data are replotted based on the work in ref. 27 (significance is indicated in P values based on Students t-test). f, Means of blood vessel and TAM product scores plotted against means of liposome tumour targeting, showing that biomarker product scoring correctly identifies breast cancers as poorly nanomedicine accumulating lesions. The error bars indicate the distribution of %ID and product score values (standard deviations on the x-axis and minima and maxima on the y-axis; n=310 as it is based on the means of c, d and e).
The liposome tumour targeting data from ref. 27 is replotted in Fig. 6e. In line with our rationale and reasoning, it can be seen that ductal breast cancer lesions in patients (5.33.0%IDkg1) accumulate radiolabelled PEGylated liposomes significantly less well than lung (18.26.6%IDkg1; P<0.05) and head and neck (33.017.6%IDkg1; P<0.05) squamous cell carcinomas. When generating tumour-tissue biomarker product scores based on the number of blood vessels and TAM per tumour type and when plotting these product scores against the average level of liposome accumulation per tumour type, we found that breast cancers clustered in the lower left corner, thereby pinpointing them as true negatives (Fig. 6f). For the majority of lung and head and neck cancer lesions, the product scores were much higher than for breast cancer, thereby classifying them as true positives. In a final validation study, we also employed the original primary tumour biopsies for biomarker assessment. For the 30 patients samples initially included, 28 primary biopsies were available. As exemplified by Figure S7, the results obtained in biopsies are very similar to those obtained in resected tumour tissues, again clearly identifying ductal breast cancers as poorly accumulating lesions. Thereby, they not only confirm the robustness of our approach but also showcase its clinical translatability. Altogether, these findings provide compelling proof-of-concept for the use of tumour blood vessels and TAM as tissue biomarkers for predicting nanomedicine tumour targeting.
Read more here:
Histopathological biomarkers for predicting the tumour accumulation of nanomedicines - Nature.com
Posted in Nano Medicine
Comments Off on Histopathological biomarkers for predicting the tumour accumulation of nanomedicines – Nature.com
Nanomedicine Market Size Expected to Reach USD 562.93 Bn by 2032 – GlobeNewswire
Ottawa, April 03, 2024 (GLOBE NEWSWIRE) -- The global nanomedicine market size was valued at USD 219.34 billion in 2023 and is predicted to hit around USD 494.62 billion by 2031, a study published by Towards Healthcare a sister firm of Precedence Research.
Report Highlights:
According to recent data, around 100+ nanomedicines have been commercially marketed, with almost 550+ nanomedicines under clinical trials.
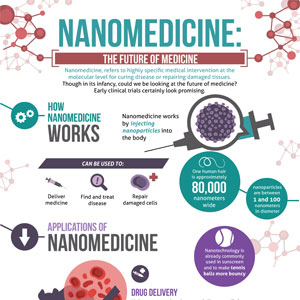
Nanomedicine involves creating and utilizing tiny structures or devices, typically between 1 and 100 nanometers in size, for medical purposes such as diagnosis and treatment. These nanoscale objects or tools, including nano-robots, skin patches, or other nanostructured materials, leverage their unique properties to achieve specific medical effects.
In medicine, nanomedicine holds promise for better drug delivery systems, more accurate imaging techniques, and even tiny devices that can target and treat diseases directly at the cellular level. Electronics enables the development of smaller and faster devices, leading to better computers, smartphones, and other gadgets.
Download a short version of this report @ https://www.towardshealthcare.com/personalized-scope/5127
Nanomedicine also has applications in energy, where it can improve the efficiency of solar panels and batteries and environmental protection, with nanomaterials being used to clean up pollutants. Nanomedicine has the potential to revolutionize many aspects of our lives, from healthcare and electronics to energy and the environment, making it a crucial area of research and innovation.
Nanomedicine is increasingly used to treat a wide range of diseases due to its ability to target specific cells or tissues precisely. In cancer treatment, nanomedicine delivers chemotherapy drugs directly to cancer cells, reducing side effects and improving effectiveness. It's also used in imaging techniques like MRI and CT scans to detect tumors early.
Additionally, nanomedicine is being explored for treating neurological disorders such as Alzheimer's and Parkinson's by delivering drugs across the blood-brain barrier and targeting diseased cells. In infectious diseases like HIV/AIDS and tuberculosis, nanomedicine can enhance drug delivery and improve the efficacy of antiviral or antibiotic medications. Furthermore, nanomedicine is being investigated for treating cardiovascular diseases, diabetes, and autoimmune disorders by developing targeted drug delivery systems and implants that regulate blood sugar levels or modulate immune responses.
Nanomedicine holds great promise in revolutionizing the treatment of various diseases by providing more effective, targeted, and less invasive therapies, potentially improving patient outcomes and quality of life.
Cancer Rates Are on the Rise
In 2022, there were about 1.92 million new cancer cases in the United States, and around 609,360 people died from cancer. Globally, this adds up to 9.6 million lives lost. Because cancer is becoming more common, we need new and better treatments. Nanomedicine is one promising way to fight cancer. It works by delivering treatments directly to cancer cells, which can make them more effective and cause fewer side effects. As more people get cancer around the world, scientists are seeing how nanomedicine could change the way we treat it. By using minimal materials and methods, researchers hope to improve cancer treatments and ease the disease's burden on society.
The rising number of individuals with cancer has led to significant growth in the nanomedicine market. This is because nanomedicine has some cool ways to help treat cancer. It helps deliver cancer drugs to the cancer cells so they work better and have fewer side effects. It improves how we see cancer using fancy imaging techniques like MRI and CT scans. This helps doctors find cancer early and treat it sooner.
You can place an order or ask any questions, please feel free to contact us at sales@towardshealthcare.com
Biomarker Detection
Biomarker detection using nanomedicine is a fancy way of saying that tiny devices and sensors can find signs of cancer in our body fluids, like blood or urine. These signs, called biomarkers, indicate whether cancer is present. These nanomedicine-based devices are super sensitive and accurate to spot even tiny amounts of these biomarkers. This helps doctors find cancer early when it's easier to treat and has a better chance of being cured.
Biomarker Detection Device for Diagnosis of Cancer
Imaging Probes:
AI-Powered Nanoparticle Bio-Detection Platform:
Not only can these nanodevices detect cancer, but they can also keep an eye on how the disease is changing over time. This helps doctors track treatment progress and see if it's working well. Plus, by predicting how cancer might respond to different treatments, these nanomedicine-based tools can help personalize treatment plans for each patient. Biomarker detection using nanomedicine is a powerful tool for early cancer detection, monitoring disease progression, and guiding treatment decisions, all of which can improve outcomes for cancer patients.
Nanomedicine lets us make personalized treatments for each person's unique cancer. That means better results and fewer problems from treatment. It helps develop new cancer therapies like heat and light therapy and boosts the body's immune system to fight cancer. Nanomedicine can spot tiny signs of cancer in our body fluids, which helps catch it early and track how it's doing during treatment. So, because more people have cancer, there's a more significant need for these intelligent nanomedicine solutions to help diagnose, treat, and keep an eye on cancer, which is making the nanomedicine market grow.
Customize this study as per your requirement @ https://www.towardshealthcare.com/customization/5127
Nanomedicines Offer Promising Advantages for Dealing with Alzheimer's
Alzheimer's disease ranked as the sixth most common cause of death in the United States, and it dropped to seventh place in both 2020 and 2021. Neurological disorders like Alzheimer's disease are becoming more common, and nanomedicine offers promising ways to manage them. In Alzheimer's, for example, the brain gets clogged with clumps of proteins, leading to memory loss and cognitive decline. Nanomedicine can help by delivering drugs directly to these protein clumps, breaking them apart and slowing down the progression of the disease.
For instance,
Additionally, nanoparticles can carry drugs across the blood-brain barrier, a protective layer around the brain that usually prevents medications from getting in. This allows for more effective treatment of neurological disorders.
Nanomedicine also enables the development of advanced imaging techniques to detect brain changes associated with neurological diseases early, allowing for timely intervention and treatment. Nanomaterials can create implants or devices that stimulate or regulate brain activity, relieving symptoms and improving the quality of life for patients with neurological disorders.
Furthermore, researchers are exploring using nanotechnology in regenerative medicine to repair damaged nerve cells and promote brain tissue regeneration. By harnessing the unique properties of nanomaterials, scientists are optimistic about the potential of nanotechnology to revolutionize the management of neurological disorders like Alzheimer's, offering hope for improved outcomes and quality of life for patients and their families.
More People Need Nanomedicine Worldwide as a Result of Advancements in Technology and Innovation
Continuous improvements in making tiny things, studying them, and simulating their behavior are pushing nanotechnology forward and making the market grow. Nanofabrication techniques are methods for building small structures, like using special machines to create tiny devices or materials. Characterization tools help us understand what these little things are made of and how they work by analyzing their properties. Simulation software allows scientists to predict how nanomaterials will behave under different conditions without physically testing them.
For instance,
All these advancements are opening up new possibilities for nanomedicine, making creating innovative products and solutions easier. For example, better nanofabrication techniques allow us to make smaller, more precise devices, while improved characterization tools help us understand how nanomaterials interact with living cells or the environment. This helps researchers develop new nanotechnology-based products for various industries, from electronics and healthcare to energy and environmental sustainability. As a result, the nanotechnology market is growing as more companies invest in developing and commercializing these advanced technologies.
Obtaining Approval for Nanomedicine Products Can Be Challenging
Getting approval for nanomedicine products can be tricky because nanoparticles behave differently than regular medicines. This makes it hard for regulators to determine their safety and effectiveness. To make things easier, we need to set up standard ways to test nanomedicine and transparent rules for how they should be regulated. This would help speed up the approval process and make it easier for these products to enter the market. Without these guidelines, it's tough for companies to get their nanomedicine products approved, which slows progress and makes it harder for patients to access these innovative treatments. Setting up clear rules and testing methods for nanomedicine is essential for getting these products out to those needing them.
A Few of the Worldwide Commercialized and FDA/EMA-Approved Formulations Based on Nanomedicines
Geographical Landscape
North America, including the United States, Canada, and Mexico, plays a significant role in nanomedicine. In the United States, many research institutions and companies work on nanomedicine. Major pharmaceutical companies invest much in nanotechnology for medicines, diagnostics, and treatments. The FDA makes sure nanomedicine products are safe and work well. Canada also does a lot of nanomedicine research. Universities, government, and companies work together on new ideas. Canadian companies focus on using nanotechnology to deliver drugs and make better medical images.
Rules in Canada make sure nanomedicine is developed and used responsibly. The North American nanomedicine market is growing because of solid funding, rules, and healthcare. More people have long-term illnesses, so there's a more significant need for new treatments. Better technology, like new ways to deliver drugs and diagnose diseases, is also helping. When academics, businesses, and government work together, it improves nanomedicine and helps it grow in North America.
Countries like China, Japan, India, and South Korea are big players in nanomedicine in the Asia-Pacific region.
For instance,
This conference aimed to share scientific advancements, industry developments, technical progress, and emerging challenges within the field of nanotechnology. They have many research centers and companies developing new nanomedicine products. Governments support these efforts with funding and initiatives. With growing healthcare needs and investments, the region is seeing rapid advancements in nanotechnology for medicine. Collaboration between countries is also helping to drive innovation and improve healthcare options.
Browse More Insights of Towards Healthcare:
Competitive Landscape
The nanomedicine market is competitive, driven by innovation, research efforts, and market demand. Big pharma, startups, and research institutions vie to develop new nanomedicines, focusing on safety, efficacy, and manufacturing. Regulatory standards shape the landscape, favoring companies that navigate them well. Partnerships and mergers bolster positions, aiding in technology access and market expansion. It's a dynamic arena marked by innovation, regulatory compliance, and collaboration, all aimed at tackling healthcare needs with advanced nanotechnology solutions.
Recent Developments
Market Key Players
Market Segmentation
By Application
By Indication
By Molecule Type
By Geography
Acquire our comprehensive analysis today @ https://www.towardshealthcare.com/price/5127
You can place an order or ask any questions, please feel free to contact us at sales@towardshealthcare.com
Explore the comprehensive statistics and insights on healthcare industry data and its associated segmentation: Get a Subscription
About Us
Towards Healthcare is a leading global provider of technological solutions, clinical research services, and advanced analytics to the healthcare sector, committed to forming creative connections that result in actionable insights and creative innovations. We are a global strategy consulting firm that assists business leaders in gaining a competitive edge and accelerating growth. We are a provider of technological solutions, clinical research services, and advanced analytics to the healthcare sector, committed to forming creative connections that result in actionable insights and creative innovations.
Web: https://www.towardshealthcare.com
Web: https://www.healthcarewebwire.com/
Browse our Brand-New Journal@ https://www.towardspackaging.com
Browse our Consulting Website@ https://www.precedenceresearch.com
For Latest Update Follow Us: https://www.linkedin.com/company/towards-healthcare
Here is the original post:
Nanomedicine Market Size Expected to Reach USD 562.93 Bn by 2032 - GlobeNewswire
Posted in Nano Medicine
Comments Off on Nanomedicine Market Size Expected to Reach USD 562.93 Bn by 2032 – GlobeNewswire
Oxford and Cardiff alumni named BSNM Champion in Nanomedicine – News from Wales
Dr. Aadarsh Mishra, 27, an alumnus of Oxford University and Cardiff University has been named as the Champion of The British Society for Nanomedicine. Aadarsh graduated with a First Class Honours in Mechanical Engineering from Cardiff University in 2017.
The British Society for Nanomedicine is the primary UK nanomedicine society which aims to raise awareness of nanomedicine research while fostering collaboration with industry, academia, clinicians and the public. The Champions of the British Society for Nanomedicine act as a local ambassador for the society, and include early career researchers, lecturers, and professors.
Aadarshs research involves rheology and biomechanical modelling of agarose gels and soft tissues. In the past, agar has been used as a multifunctional encapsulating material and as a drug carrier. Aadarsh has been particularly working with agarose hydrogels and investigating their biomechanical properties as a soft tissue mimic. His work will lead to a better understanding of the agarose-tissue response in time and frequency domain. During his research, Aadarsh has mimicked heart and kidney tissues using agarose hydrogels which will have potential applications in elastography techniques such as Magnetic Resonance Elastography (MRE), Acoustic Radiation Force Impulse Imaging (ARFI) and Shear Wave Elastography (SWE). Moreover, the agarose mimicking kidney will have potential applications during lithotripsy technique (for kidney stone treatment).
Aadarsh worked with Alesi Surgical Ltd. (Cardiff) as a Research and Development (R&D) Engineer (from 2015-17) and co-invented the design electrode shield which was later filed as an international patent. At the age of 21, Aadarsh co-authored a high-impact factor paper in Nano Letters (published by American Chemical Society) where he performed Finite Element Analysis (FEA) simulations. Aadarsh has also worked at the Indian Institute of Technology (IIT Delhi) on a defence project where he was developing experimental setups for high strain rate testing. In 2014, Aadarsh pursued his research internship at the Indian Institute of Science (IISc, Bangalore) on a project related to Tribology.
Aadarsh has also published a chapter in the book Power Ultrasonics and presented his work at several international conferences such as Annual European Rheology Conference and 18th European Mechanics of Materials Conference. Aadarsh was also elected as the Fellow of Royal Astronomical Society at 19 years of age.
See the article here:
Oxford and Cardiff alumni named BSNM Champion in Nanomedicine - News from Wales
Posted in Nano Medicine
Comments Off on Oxford and Cardiff alumni named BSNM Champion in Nanomedicine – News from Wales
Understanding the Protein Corona in Nanomedicine – Medriva
Understanding the Protein Corona in Nanomedicine
As nanomedicine continues to expand its horizons in the field of therapeutic nucleic acid delivery and beyond, understanding the protein corona, a layer of biomolecules that forms on nanoparticles in biological fluids, is of critical importance. This protein layer plays a pivotal role in determining the safety and efficacy of nanomedicine.
A recent multi-center study involving 17 proteomics facilities underscored the significance of this layer, revealing substantial data variability. Remarkably, only 1.8% of proteins were consistently identified across these centers, indicating the need for a harmonized approach to nanoparticle protein corona analysis.
The study further illuminated the importance of standardizing procedures in protein corona analysis. The implementation of an aggregated database search with uniform parameters proved instrumental in harmonizing proteomics data, increasing the reproducibility and the percentage of consistently identified unique proteins across distinct cores.
More specifically, the study found that reduction and alkylation are crucial steps in protein corona sample processing, with the omission of these steps reducing the number of total quantified peptides by around 20%. Thus, uniform data processing pipelines can play a major role in enhancing the reproducibility of protein corona analysis.
Just like plasma proteomics, protein corona analysis faces an array of challenges, including a broad dynamic range and the presence of different protein isoforms. Furthermore, the composition of the protein corona determines how biosystems perceive nanoparticles, a factor that can lead to biased data interpretation if low-abundant genuine targets are not detected. The quality and proteome coverage of protein corona reported by core facilities can be affected by various factors, further underscoring the need for standardization across different proteomics studies.
The study also investigated the influence of database search, data extraction, processing, and analysis on observed data heterogeneity, laying the groundwork for future research to standardize and harmonize results. This is particularly important in the realm of nanomedicine, where protein-based nanoparticles show immense potential for therapeutic nucleic acid delivery, owing to their unique properties such as biodegradability, biocompatibility, and ease of functionalization.
Looking forward, the standardization and harmonization of protein corona data will be instrumental in overcoming barriers to effective protein nanoparticle-mediated nucleic acid delivery. It will also aid in the development of non-viral protein materials for nucleic acid delivery, and in the design of smart drug delivery systems (DDS) that specifically target pathologic tissues while minimizing off-target effects on healthy tissues.
By addressing these challenges and advancing clinical applications of nanoscale biotechnologies, we may be one step closer to realizing the full potential of nanomedicine, from insulin injections and treatment of rheumatoid arthritis to monitoring oxygen levels and overcoming barriers to nanoparticle penetration into tumors.
Continued here:
Understanding the Protein Corona in Nanomedicine - Medriva
Posted in Nano Medicine
Comments Off on Understanding the Protein Corona in Nanomedicine – Medriva