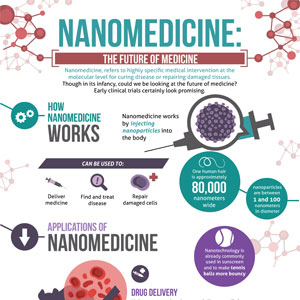
Nanomedicine is the medical application of nanotechnology.[1] Nanomedicine ranges from the medical applications of nanomaterials, to nanoelectronic biosensors, and even possible future applications of molecular nanotechnology. Current problems for nanomedicine involve understanding the issues related to toxicity and environmental impact of nanoscale materials (materials whose structure is on the scale of nanometers, i.e. billionths of a meter).
Functionalities can be added to nanomaterials by interfacing them with biological molecules or structures. The size of nanomaterials is similar to that of most biological molecules and structures; therefore, nanomaterials can be useful for both in vivo and in vitro biomedical research and applications. Thus far, the integration of nanomaterials with biology has led to the development of diagnostic devices, contrast agents, analytical tools, physical therapy applications, and drug delivery vehicles.
Nanomedicine seeks to deliver a valuable set of research tools and clinically useful devices in the near future.[2][3] The National Nanotechnology Initiative expects new commercial applications in the pharmaceutical industry that may include advanced drug delivery systems, new therapies, and in vivo imaging.[4] Nanomedicine research is receiving funding from the US National Institutes of Health, including the funding in 2005 of a five-year plan to set up four nanomedicine centers.
Nanomedicine is a large industry, with nanomedicine sales reaching $6.8 billion in 2004, and with over 200 companies and 38 products worldwide, a minimum of $3.8 billion in nanotechnology R&D is being invested every year.[5] In April 2006, the journal Nature Materials estimated that 130 nanotech-based drugs and delivery systems were being developed worldwide.[6] As the nanomedicine industry continues to grow, it is expected to have a significant impact on the economy.
Nanotechnology has provided the possibility of delivering drugs to specific cells using nanoparticles.
The overall drug consumption and side-effects may be lowered significantly by depositing the active agent in the morbid region only and in no higher dose than needed. Targeted drug delivery is intended to reduce the side effects of drugs with concomitant decreases in consumption and treatment expenses. Drug delivery focuses on maximizing bioavailability both at specific places in the body and over a period of time. This can potentially be achieved by molecular targeting by nanoengineered devices.[7][8] More than $65 billion are wasted each year due to poor bioavailability.[citation needed] A benefit of using nanoscale for medical technologies is that smaller devices are less invasive and can possibly be implanted inside the body, plus biochemical reaction times are much shorter. These devices are faster and more sensitive than typical drug delivery.[9] The efficacy of drug delivery through nanomedicine is largely based upon: a) efficient encapsulation of the drugs, b) successful delivery of drug to the targeted region of the body, and c) successful release of the drug.[citation needed]
Drug delivery systems, lipid- [10] or polymer-based nanoparticles,[11] can be designed to improve the pharmacokinetics and biodistribution of the drug.[12][13][14] However, the pharmacokinetics and pharmacodynamics of nanomedicine is highly variable among different patients.[15] When designed to avoid the body's defence mechanisms,[16] nanoparticles have beneficial properties that can be used to improve drug delivery. Complex drug delivery mechanisms are being developed, including the ability to get drugs through cell membranes and into cell cytoplasm. Triggered response is one way for drug molecules to be used more efficiently. Drugs are placed in the body and only activate on encountering a particular signal. For example, a drug with poor solubility will be replaced by a drug delivery system where both hydrophilic and hydrophobic environments exist, improving the solubility.[17] Drug delivery systems may also be able to prevent tissue damage through regulated drug release; reduce drug clearance rates; or lower the volume of distribution and reduce the effect on non-target tissue. However, the biodistribution of these nanoparticles is still imperfect due to the complex host's reactions to nano- and microsized materials[16] and the difficulty in targeting specific organs in the body. Nevertheless, a lot of work is still ongoing to optimize and better understand the potential and limitations of nanoparticulate systems. While advancement of research proves that targeting and distribution can be augmented by nanoparticles, the dangers of nanotoxicity become an important next step in further understanding of their medical uses.[18]
Nanoparticles can be used in combination therapy for decreasing antibiotic resistance or for their antimicrobial properties.[19][20][21] Nanoparticles might also used to circumvent multidrug resistance (MDR) mechanisms.[22]
Two forms of nanomedicine that have already been tested in mice and are awaiting human trials that will be using gold nanoshells to help diagnose and treat cancer,[23] and using liposomes as vaccine adjuvants and as vehicles for drug transport.[24][25] Similarly, drug detoxification is also another application for nanomedicine which has shown promising results in rats.[26] Advances in Lipid nanotechnology was also instrumental in engineering medical nanodevices and novel drug delivery systems as well as in developing sensing applications.[27] Another example can be found in dendrimers and nanoporous materials. Another example is to use block co-polymers, which form micelles for drug encapsulation.[11]
Polymeric nano-particles are a competing technology to lipidic (based mainly on Phospholipids) nano-particles. There is an additional risk of toxicity associated with polymers not widely studied or understood. The major advantages of polymers is stability, lower cost and predictable characterisation. However, in the patient's body this very stability (slow degradation) is a negative factor. Phospholipids on the other hand are membrane lipids (already present in the body and surrounding each cell), have a GRAS (Generally Recognised As Safe) status from FDA and are derived from natural sources without any complex chemistry involved. They are not metabolised but rather absorbed by the body and the degradation products are themselves nutrients (fats or micronutrients).
The rest is here:
Nanomedicine - Wikipedia, the free encyclopedia
Recommendation and review posted by Guinevere Smith